10 Ocak 2016 Pazar
Biocompatibility
Biocompatibility is related to the behavior of biomaterials in various contexts. The term refers to the ability of a material to perform with an appropriate host response in a specific situation.The ambiguity of the term reflects the ongoing development of insights into how biomaterials interact with the human body and eventually how those interactions determine the clinical success of a medical device (such as pacemaker, hip replacement or stent). Modern medical devices and prostheses are often made of more than one material so it might not always be sufficient to talk about the biocompatibility of a specific material.
Indeed, since the immune response and repair functions in the body are so complicated it is not adequate to describe the biocompatibility of a single material in relation to a single cell type or tissue. Sometimes one hears of biocompatibility testing that is a large battery of in vitro test that is used in accordance with ISO 10993 (or other similar standards) to determine if a certain material (or rather biomedical product) is biocompatible. These tests do not determine the biocompatibility of a material, but they constitute an important step towards the animal testing and finally clinical trials that will determine the biocompatibility of the material in a given application, and thus medical devices such as implants or drug delivery devices.
Surgical Suture
All sutures are classified as either absorbable or non-absorbable depending on whether the body will naturally degrade and absorb the suture material over time.
Absorbable suture materials include the original catgut as well as the newer synthetics polyglycolic acid, polylactic acid, polydioxanone, and caprolactone. They are broken down by various processes including hydrolysis (polyglycolic acid) and proteolytic enzymatic degradation. Depending on the material, the process can be from ten days to eight weeks. They are used in patients who cannot return for suture removal, or in internal body tissues. In both cases, they will hold the body tissues together long enough to allow healing, but will disintegrate so that they do not leave foreign material or require further procedures. Occasionally, absorbable sutures can cause inflammation and be rejected by the body rather than absorbed
Non-absorbable sutures are made of special silk or the synthetics polypropylene, polyester or nylon. Stainless steel wires are commonly used in orthopedic surgery and for sternal closure in cardiac surgery. These may or may not have coatings to enhance their performance characteristics. Non-absorbable sutures are used either on skin wound closure, where the sutures can be removed after a few weeks, or in stressful internal environments where absorbable sutures will not suffice. Examples include the heart (with its constant pressure and movement) or the bladder (with adverse chemical conditions). Non-absorbable sutures often cause less scarring because they provoke less immune response, and thus are used where cosmetic outcome is important. They may be removed after a certain time, or left permanently.
Non-absorbable sutures are made of special silk or the synthetics polypropylene, polyester or nylon. Stainless steel wires are commonly used in orthopedic surgery and for sternal closure in cardiac surgery. These may or may not have coatings to enhance their performance characteristics. Non-absorbable sutures are used either on skin wound closure, where the sutures can be removed after a few weeks, or in stressful internal environments where absorbable sutures will not suffice. Examples include the heart (with its constant pressure and movement) or the bladder (with adverse chemical conditions). Non-absorbable sutures often cause less scarring because they provoke less immune response, and thus are used where cosmetic outcome is important. They may be removed after a certain time, or left permanently.
Stents
In medicine, a stent is a tube or other device placed in the body to create a passage between two hollow spaces, and stenting is the placement of a stent. There is a wide variety of stents used for different purposes, from expandable coronary, vascular and biliary stents, to simple plastic stents used to allow the flow of urine between kidney and bladder.
Breast implant
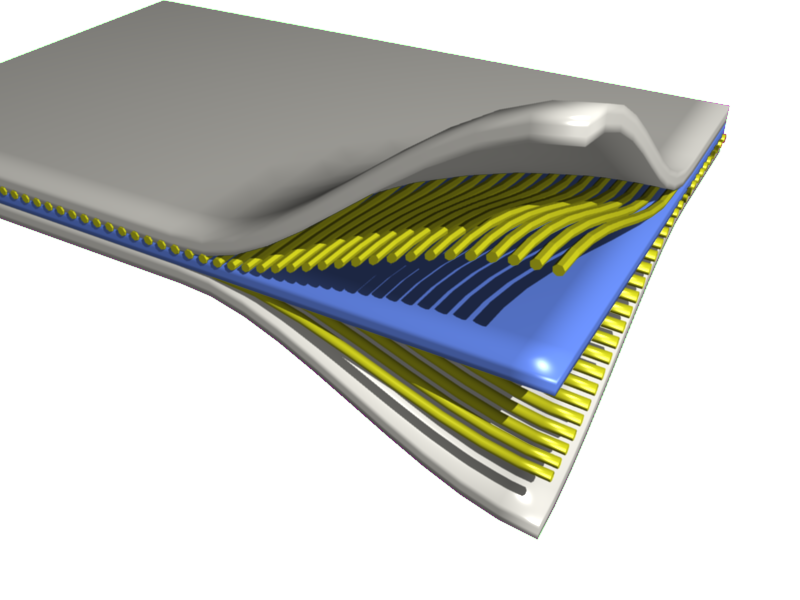
A Breast İmplant is a prosthesis used to change the size, shape, and contour of a woman’s breast. In reconstructive plastic surgery, breast implants can be placed to restore a natural looking breast mound for post–mastectomy breast reconstruction patients or to correct congenital defects and deformities of the chest wall. They are also used cosmetically to enhance or enlarge the appearance of the breast through breast augmentation surgery.
There are three general types of breast implant devices, defined by their filler material: saline solution, silicone gel, and composite filler. The saline implant has an elastomer silicone shell filled with sterile saline solutionduring surgery; the silicone implant has an elastomer silicone shell pre-filled with viscous silicone gel; and the alternative composition implants featured miscellaneous fillers, such as soy oil, polypropylene string, etc. Composite implants are typically not recommended for use anymore and, in fact, their use is banned in the United States and Europe due to associated health risks and complications.
In surgical practice, for the reconstruction of a breast, the tissue expander device is a temporary breast prosthesis used to form and establish an implant pocket for the future permanent breast implant. For the correction of male breast defects and deformities, the pectoral implant is the breast prosthesis used for the reconstruction and the aesthetic repair of a man’s chest wall.
Contact Lenses
A Contact Lens, or simply contact, is a thin lens placed directly on the surface of the eye. Contact lenses are considered medical devices and can be worn to correct vision, or for cosmetic or therapeutic reasons.In 2004, it was estimated that 125 million people (2%) use contact lenses worldwide, including 28 to 38 million in the United States. In 2010, worldwide contact lens market was estimated at $6.1 billion, while the U.S. soft lens market is estimated at $2.1 billion. Multiple scientists have estimated that the global market will reach $11.7 billion by 2015.As of 2010, the average age of contact lens wearers globally was 31 years old and two thirds of wearers were female.
People choose to wear contact lenses for many reasons. Aesthetics and cosmetics are often motivating factors for people who would like to avoid wearing glasses or would like to change the appearance of their eyes.Other people wear contacts for functional or optical reasons. When compared with spectacles, contact lenses typically provide better peripheral vision, and do not collect moisture such as rain, snow, condensation, or sweat (extreme weather). This makes them ideal for sports and other outdoor activities. Contact lens wearers can also wear sunglasses, goggles, or other eyewear of their choice without having to fit them with prescription lenses or worry about compatibility with glasses. Additionally, there are conditions such as keratoconus and aniseikonia that are typically corrected better by contacts than by glasses.
Heart Valve
An artificial heart valve is a device implanted in the heart of a patient with valvular heart disease.When one of the four heart valves malfunctions, the medical choice may be to replace the natural valve with an artificial valve. This requires open-heart surgery.
Valves are integral to the normal physiological functioning of the human heart. Natural heart valves are evolved to forms that perform the functional requirement of inducing unidirectional blood flow through the valve structure from one chamber of the heart to another. Natural heart valves become dysfunctional for a variety of pathological causes. Some pathologies may require complete surgical replacement of the natural heart valve with a heart valve prosthesis.
Dental İmplant
A Dental implant (also known as an endosseous implant or fixture) is a surgical component that interfaces with the bone of the jaw or skull to support a dental prosthesis such as a crown, bridge, denture, facial prosthesis or to act as an orthodontic anchor. The basis for modern dental implants is a biologic process called osseointegration where materials, such as titanium, form an intimate bond to bone. The implant fixture is first placed, so that it is likely to osseointegrate, then a dental prosthetic is added. A variable amount of healing time is required for osseointegration before either the dental prosthetic (a tooth, bridge or denture) is attached to the implant or an abutment is placed which will hold a dental prosthetic.
Success or failure of implants depends on the health of the person receiving it, drugs which impact the chances of osseointegration and the health of the tissues in the mouth. The amount of stress that will be put on the implant and fixture during normal function is also evaluated. Planning the position and number of implants is key to the long-term health of the prosthetic since biomechanical forces created during chewing can be significant. The position of implants is determined by the position and angle of adjacent teeth, lab simulations or by using computed tomography with CAD/CAM simulations and surgical guides called stents. The prerequisites to long-term success of osseointegrated dental implants are healthy bone and gingiva. Since both can atrophy after tooth extraction pre-prosthetic procedures, such as sinus lifts or gingival grafts, are sometimes required to recreate ideal bone and gingiva.
The final prosthetic can be either fixed, where a person cannot remove the denture or teeth from their mouth or removable, where they can remove the prosthetic. In each case an abutment is attached to the implant fixture. Where the prosthetic is fixed, the crown, bridge or denture is fixed to the abutment with either lag screws or dental cement. Where the prosthetic is removable, a corresponding adapter is placed in the prosthetic so that the two pieces can be secured together.
The risks and complications related to implant therapy are divided into those that occur during surgery (such as excessive bleeding or nerve injury), those that occur in the first six months (such as infection and failure to osseointegrate) and those that occur long-term (such as peri-implantitis and mechanical failures). In the presence of healthy tissues, a well integrated implant with appropriate biomechanical loads can have 5-year plus survival rates from 93 to 98 percent. and 10 to 15 year lifespans for the prosthetic teeth.
Bone Cement
Bone cements have been used very successfully to anchor artificial joints (hip joints, knee joints, shoulder and elbow joints) for more than half a century. Artificial joints (referred to as prostheses) are anchored with bone cement. The bone cement fills the free space between the prosthesis and the bone and plays the important role of an elastic zone. This is necessary because the human hip is acted on by approximately 10-12 times the body weight and therefore the bone cement must absorb the forces acting on the hips to ensure that the artificial implant remains in place over the long term.
Bone cement chemically is nothing more than Plexiglas (i.e. polymethyl methacrylate or PMMA). PMMA was used clinically for the first time in the 1940s in plastic surgery to close gaps in the skull. Comprehensive clinical tests of the compatibility of bone cements with the body were conducted before their use in surgery. The excellent tissue compatibility of PMMA allowed bone cements to be used for anchorage of head prostheses in the 1950s.
Today several million procedures of this type are conducted every year all over the world and more than half of them routinely use bone cements - and the proportion is increasing. Bone cement is considered a reliable anchorage material with its ease of use in clinical practice and particularly because of its proven long survival rate with cemented-in prostheses. Hip and knee registers for artificial joint replacements such as those in Sweden and Norway clearly demonstrate the advantages of cemented-in anchorage. A similar register for endoprosthesis was introduced in Germany in 2010.
Joint Replacement
Replacement arthroplasty (from Greek arthron, joint, limb, articulate, + plassein, to form, mould, forge, feign, make an image of), or joint replacement surgery, is a procedure of orthopedic surgery in which an arthritic or dysfunctional joint surface is replaced with an orthopedic prosthesis. Joint replacement is considered as a treatment when severe joint pain or dysfunction is not alleviated by less-invasive therapies. During the latter half of the 20th century, rheumasurgery developed as a subspecialty focused on these and a few other procedures in patients with rheumatic diseases.
Joint replacement surgery is becoming more common with knees and hips replaced most often. About 773,000 Americans had a hip or knee replaced in 2009.
Titanium carbide has proved to be possible to use combined with sintered polycrystalline diamond surface (PCD), a superhard ceramic which promises to provide an improved, strong, long-wearing material for artificial joints. PCD is formed from polycrystalline diamond compact (PDC) through a process involving high pressures and temperatures. When compared with other ceramic materials such as cubic boron nitride, silicon nitride, and aluminum oxide, PCD shows many better characteristics, including a high level of hardness and a relatively low coefficient of friction. For the application of artificial joints it will likely be combined with certain metals and metal alloys like cobalt, chrome, titanium, vanadium, stainless steel, aluminum, nickel, hafnium, silicon, cobalt-chrome, tungsten, zirconium, etc. This means that people with nickel allergy or sensitivities to other metals are at risk for complications due to the chemicals in the device.
In joints such as knee replacements there are two parts that are ceramic and they can be made of either the same ceramic or a different one. If they are made of the same ceramic, however, they have different weight ratios. These ceramic parts are configured so that should shards break off of the implant, the particles are benign and not sharp. They are also made so that if a shard were to break off of one of the two ceramic components, they would be noticeable through x-rays during a check-up or inspection of the implant. With implants such as hip implants, the ball of the implant could be made of ceramic, and between the ceramic layer and where it attaches to the rest of the implant, there is usually a membrane to help hold the ceramic. The membrane can help prevent cracks, but if cracks should occur at two points which create a separate piece, the membrane can hold the shard in place so that it doesn't leave the implant and cause further injury. Because these cracks and separations can occur, the material of the membrane is a bio-compatible polymer that has a high fracture toughness and a high shear toughness.
Applications of Biomaterials
- Joint replacements
- Bone plates
- Bone cement
- Artificial ligaments and tendons
- Dental implants for tooth fixation
- Blood vessel prostheses
- Heart valves
- Skin repair devices (artificial tissue)
- Cochlear replacements
- Contact lenses
- Breast implants
- Drug delivery mechanisms
- Sustainable materials
- Vascular grafts
- Stents
- Nerve conduits
- Surgical sutures
Structural Hierarchy
Nearly all materials could be seen as hierarchically structured, especially since the changes in spatial scale bring about different mechanisms of deformation and damage. However, in biological materials this hierarchical organization is inherent to the microstructure. One of the first examples of this, in the history of structural biology, is the early X-Ray scattering work on the hierarchical structure of hair and wool by Astbury and Woods. In bone, for example, collagen is the building block of the organic matrix—a triple helix with diameter of 1.5 nm. These tropocollagen molecules are intercalated with the mineral phase (hydroxyapatite, a calcium phosphate) forming fibrils that curl into helicoids of alternating directions. These "osteons" are the basic building blocks of bones, with the volume fraction distribution between organic and mineral phase being about 60/40.
In another level of complexity, the hydroxyapatite crystals are platelets that have a diameter of approximately 70–100 nm and thickness of 1 nm. They originally nucleate at the gaps between collagen fibrils.
Similarly, the hierarchy of abalone shell begins at the nanolevel, with an organic layer having a thickness of 20–30 nm. This layer proceeds with single crystals of aragonite (a polymorph of CaCO3) consisting of "bricks" with dimensions of 0.5 and finishing with layers approximately 0.3 mm (mesostructure).
Crabs are arthropods whose carapace is made of a mineralized hard component (which exhibits brittle fracture) and a softer organic component composed primarily of chitin. The brittle component is arranged in a helical pattern. Each of these mineral ‘rods’ ( 1 μm diameter) contains chitin–protein fibrils with approximately 60 nm diameter. These fibrils are made of 3 nm diameter canals which link the interior and exterior of the shell.
Self-Assembly
Self-assembly is the most common term in use in the modern scientific community to describe the spontaneous aggregation of particles (atoms, molecules, colloids, micelles, etc.) without the influence of any external forces. Large groups of such particles are known to assemble themselves into thermodynamically stable, structurally well-defined arrays, quite reminiscent of one of the 7 crystal systems found in metallurgy and mineralogy (e.g. face-centered cubic, body-centered cubic, etc.). The fundamental difference in equilibrium structure is in the spatial scale of the unit cell (or lattice parameter) in each particular case.
Molecular self-assembly is found widely in biological systems and provides the basis of a wide variety of complex biological structures. This includes an emerging class of mechanically superior biomaterials based on microstructural features and designs found in nature. Thus, self-assembly is also emerging as a new strategy in chemical synthesis and nanotechnology. Molecular crystals, liquid crystals, colloids, micelles, emulsions, phase-separated polymers, thin films and self-assembled monolayers all represent examples of the types of highly ordered structures which are obtained using these techniques. The distinguishing feature of these methods is self-organization.
Biomineralization
Biomineralization is the process by which living organisms produce minerals,often to harden or stiffen existing tissues. Such tissues are called mineralized tissues. It is an extremely widespread phenomenon; all six taxonomic kingdoms contain members that are able to form minerals, and over 60 different minerals have been identified in organisms.Examples include silicates in algae and diatoms, carbonates in invertebrates, and calcium phosphates and carbonates in vertebrates. These minerals often form structural features such as sea shells and the bone in mammals and birds. Organisms have been producing mineralised skeletons for the past 550 million years. Other examples include copper, iron and gold deposits involving bacteria.
Biologically-formed minerals often have special uses such as magnetic sensors in magnetotactic bacteria (Fe3O4), gravity sensing devices (CaCO3, CaSO4, BaSO4) ,biomaterials, iron storage and mobilization (Fe2O3•H2O in the protein ferritin).
Composite Material
Composite material (also called a composition material or shortened to composite) is a material made from two or more constituent materials with significantly different physical or chemical properties that, when combined, produce a material with characteristics different from the individual components. The individual components remain separate and distinct within the finished structure. The new material may be preferred for many reasons: common examples include materials which are stronger, lighter, or less expensive when compared to traditional materials. More recently, researchers have also begun to actively include sensing, actuation, computation and communication into composites,which are known as Robotic Materials.
What is Biomaterial?
The study of biomaterials is called biomaterials science or biomaterials engineering. It has experienced steady and strong growth over its history, with many companies investing large amounts of money into the development of new products. Biomaterials science encompasses elements of medicine, biology, chemistry, tissue engineering and materials science.
What is Material?
Material is a broad term for the (chemical) substance, or a mixture of substances that constitute a thing.Materials can be in various forms and can have different features.
There are five types of material:
1-)Biomaterial
2-)Raw material
3-)Textile Materials
4-)Composite Material
Kaydol:
Yorumlar (Atom)